
The anterior cruciate ligament (ACL) is one of four major stabilising knee ligaments that connect the femur or thigh bone to the tibia or shin bone. The ligament is a very important part of the knee joint. Injuries can occur from a bad tackle during football or rugby, or a sharp sudden twisting movement. It can also be damaged from jumping and landing awkwardly.
ACL tears are typically ruptures, so the whole ligament is compromised. Initially you will have gross swelling in your knee joint, followed by gross stiffness and you will be unable to walk. As weeks progress, walking will improve and the swelling will reduce, and after several months your knee can be left unstable and prone to giving way.
Surgical Options
The aim of surgical intervention is restoration of ACL function in order to prevent knee instability.
The torn ACL is usually reconstructed by arthroscopic surgery. The injured ligament is replaced by a graft made of tendon. The most commonly used grafts include: patellar tendon, hamstring tendon and quadriceps tendon.
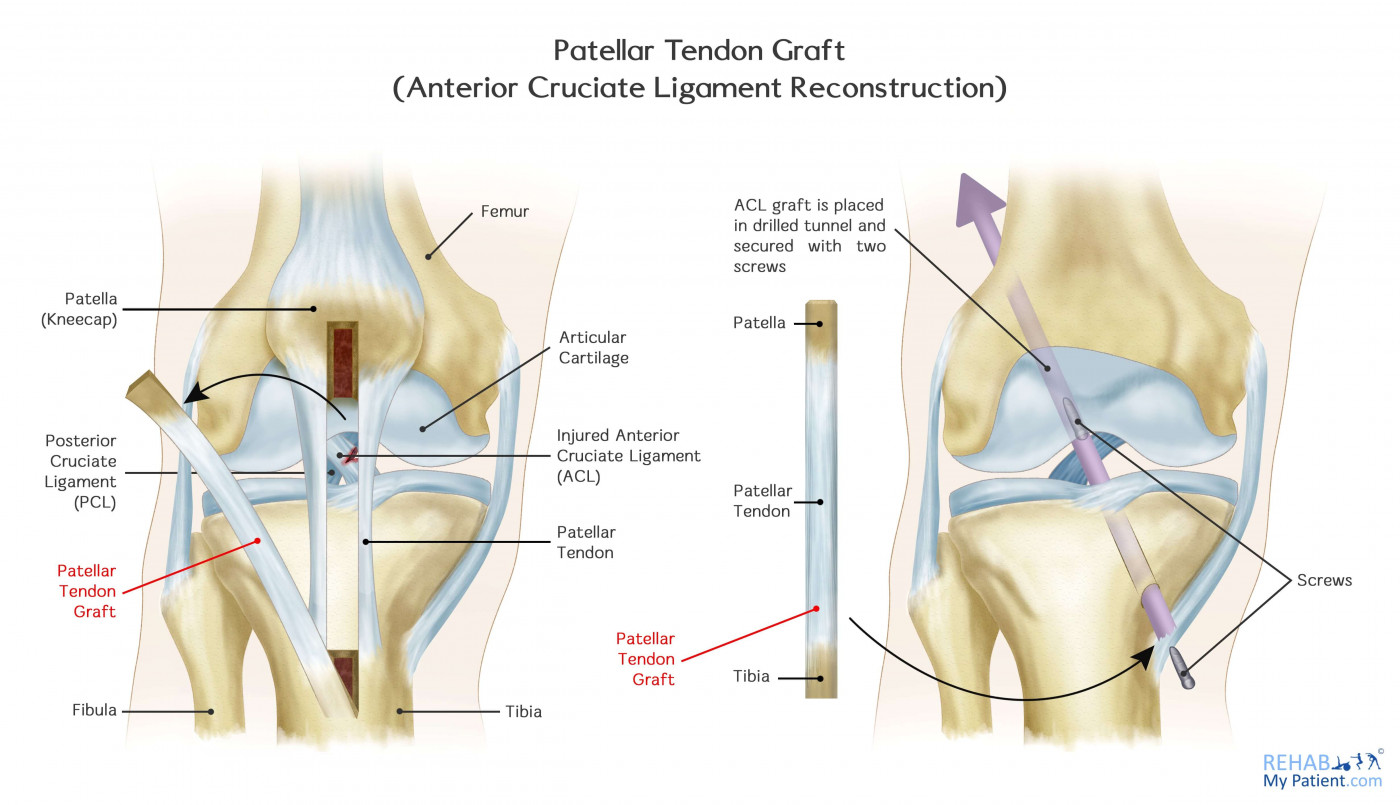
Patellar Tendon Graft
The patellar tendon is located on the front of your knee and connects the knee cap or patella to the shin bone or tibia. The tendon graft consists of the central third of the patellar tendon with a bone plug on either side of the tendon graft.
Advantages:
- Resembles the ACL in length
- The bone ends of the graft are positioned in the bone where the ACL attaches. In such way, “bone to bone” healing occurs which is considered as strong healing method
Disadvantages:
- Increased risk of patellar fracture due to removal of bone from the knee cap when graft is taken
- Postoperative pain behind the knee cap
- Pain with kneeling, even years after surgery
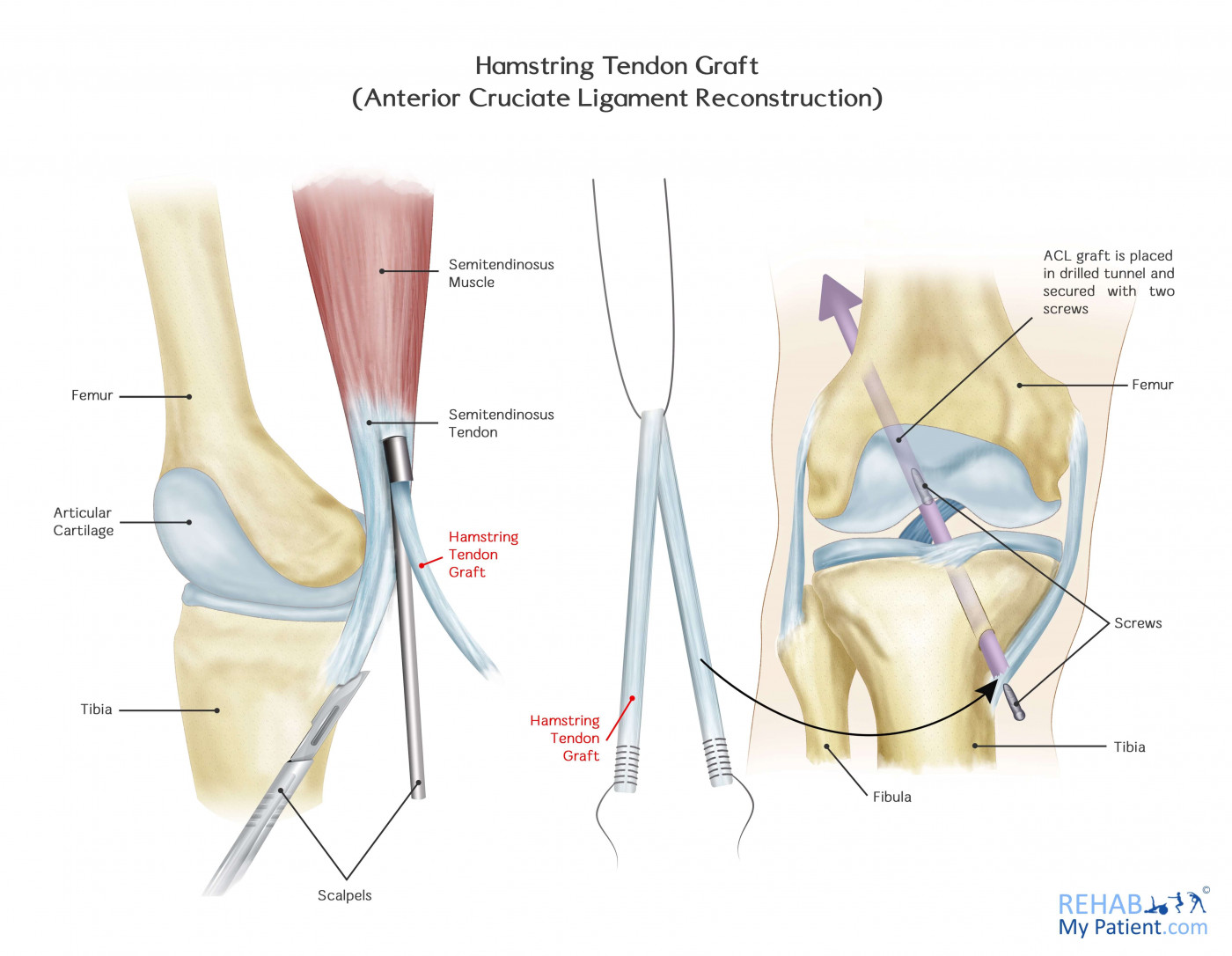
Hamstring Tendon Graft
The hamstring muscles are the group of muscles positioned on the back of your thigh. The hamstring tendon autograft is formed by two of the tendons of these muscles (usually semitendinosus and gracilis). The tendons are united in order to create a new ACL.
Advantages:
- Less postoperative pain and stiffness compared to patellar tendon graft
- Incision site is smaller
Disadvantages:
- Compared to patellar tendon graft, healing is slower as there is no “bone to bone” healing. The hamstring graft requires a longer period of time to become rigid.
Quadriceps Tendon Graft
This type of graft is used when previous ACL reconstruction fails. The middle third of the quadriceps tendon is removed together with a bone plug from the patella (knee cap). It is commonly used for taller and heavier patients. Main disadvantages include not so solid fixation compared to the patellar tendon graft and high risk of postoperative pain in the knee cap. Additionally, the incision tends to be big and not cosmetically appealing.
Tips for Recovery/Rehabilitation
Rehabilitation is one of the most important, yet often neglected, aspect of ACL reconstruction surgery. Exercises and rehab are a crucial part of successful ACL surgery and much of its success depends on the patient’s dedication to rigorous physical therapy and home exercise programs.
Some basic recommendations for recovering quickly from ACL surgery include the following. Patients who follow them tend to have a better surgical outcome and a faster recovery than patients who don't.
- Follow post-op instructions: Immediately after ACL surgery, you will most likely receive specific instructions from your surgeon and then meet with a physical therapist to establish an ACL rehabilitation programme.
- Get a referral for to see your therapist: Physical therapy is generally prescribed after ACL surgery. If you don't receive a referral to PT, ask your surgeon for one.
- Go to your follow up appointments: It's important that your progress is monitored and your plan readjusted, if needed.
- Perform the prescribed exercises: Your physical therapist will determine your rehab programme based upon your personal limitations and set your exercise progression based upon your improvement. Again, for the best outcome, it's important to follow this program exactly.
- Get proper nutrition: Eating well after surgery can help your body heal faster. Recommended foods include lean protein (red meat, chicken or fish), dairy, and fresh citrus. Vegetables are nutrient-rich, so eat plenty of green leafy plants. Many nutritionists recommend stopping or at least limiting caffeine, alcohol and sodas.
- Get enough sleep: While you sleep, your body repairs tissues and promotes healing, so be sure to get at least eight hours of quality sleep every night.
- Take medication as prescribed
- Inform your surgeon of changes in your recovery: If your pain suddenly increases, you develop a fever or other symptoms of infection, it's important to let your doctor know immediately.
- Ask for help: After surgery, you will be less mobile and will probably need additional help with daily activities. Don't be afraid to ask for help from your relatives and friends.
Sign Up
Sign up for your free trial now!
Get started with Rehab My Patient today and revolutionize your exercise prescription process for effective rehabilitation.
Start Your 14-Day Free Trial