
Diabetes is a condition where the blood sugar levels are elevated in about 6 percent of those within the US, which equates to roughly 16 million individuals. Diabetes is also rapidly growing in other Western countries, Europe and Africa. Diabetic foot conditions are one of the main health concerns for these individuals and can in some cases require the individual to be hospitalized.
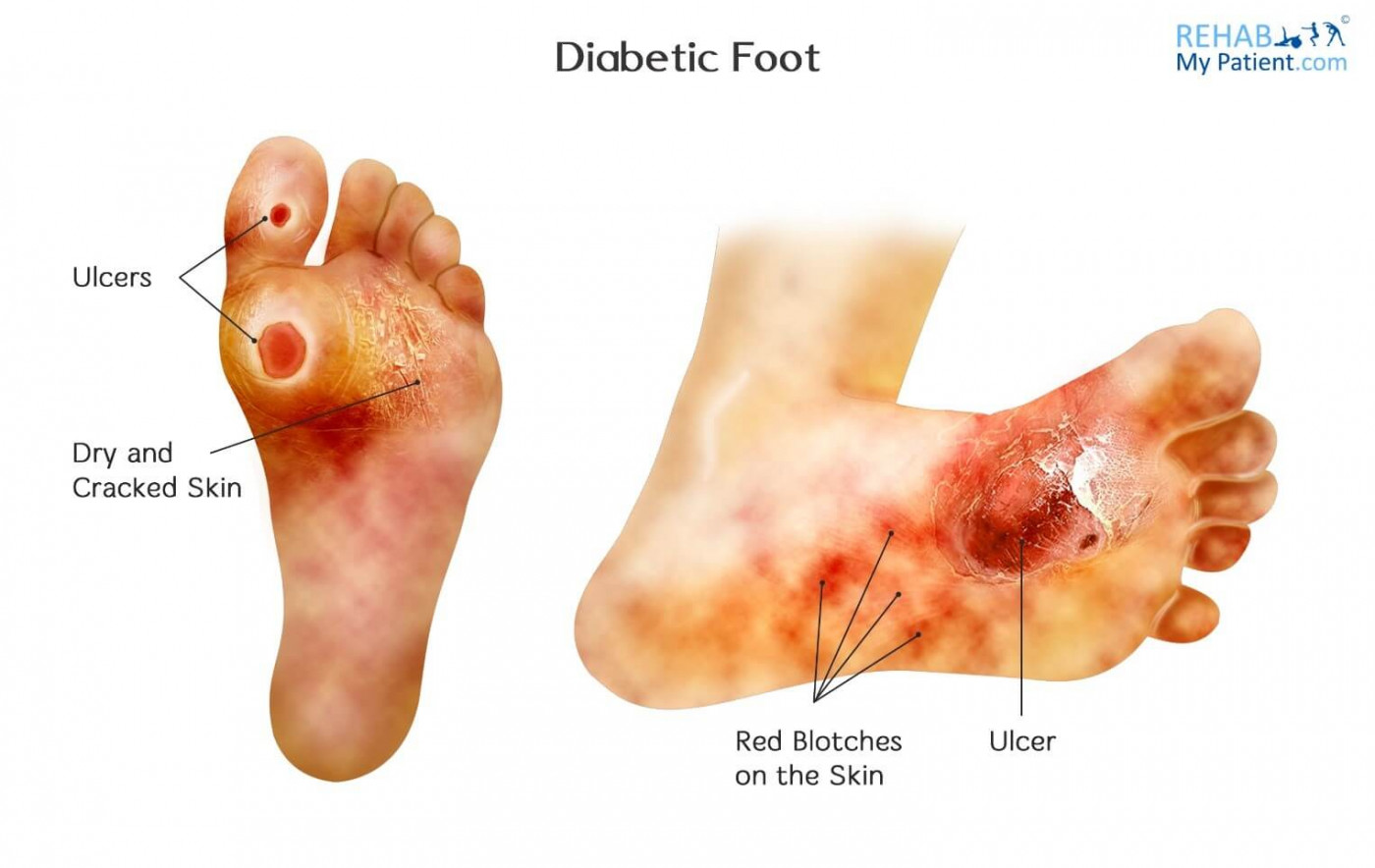
Most of the foot problems for those who have diabetes arise from two severe complications of the disease: poor circulation and nerve damage. The poor circulation actually causes the nerve damage. One of the main critical problems that these complications can create is Charcot arthropathy, which deforms the foot’s shape and cause disability.
Treatment options are available for this specific condition, but the most effective is that of prevention. For those who are suffering with diabetes, careful inspections on a daily basis of the feet is imperative to the overall health and well-being and preventing potential foot problems in individuals.
Diabetic Foot Anatomy
Diabetes is known to cause damage to the blood vessels in individuals, which decreases blood flow to the feet. If poor circulation occurs, the bones are weakened and the joints and bones of the ankle and foot disintegrate. For those who have diabetes, there is an increased risk of broken bones in the foot.
How to Treat Diabetic Foot:
- Casting
In the early stages of the condition, it can often be treated with a cast or boot to help protect the ankle and the foot. Using a cast is quite effective in minimizing the amount of swelling and helping to protect the bones. Casting requires that the individual doesn’t put any weight onto the foot until after the bones have begun to heal. Healing will often take three months or more. Every week to two weeks the cast is changed to make sure it still fits as the swelling is minimized.
- Custom Shoes
Once the initial swelling has decreased and the bones are able to fuse together again, specialized shoes or walking boots might be needed. This show is designed to help decrease the likelihood of ulcers from occurring. Some diabetics aren’t able to wear traditional shoes because they won’t fit the deformed foot properly.
- Surgery
If the deformity is putting the patient at risk for ulcers and wearing the protective shoes isn’t work, surgery might be the only alternative. Dislocations and unstable fractures will need surgery for them to heal properly. Various types of deformities exist, so the treatment options will vary as well.
Tips:
- Adhere to the instructions provided from your health care provider in terms of when it is safe to put weight back onto the injured foot.
- The sooner the condition is treated and diagnosed, the better the end result is going to be.
- Patients need to take the time to examine the feet on a daily basis and keep blood sugar levels in check.
- Be on the lookout for redness, swelling and other changes to the foot that you haven’t noticed previously.
- Swelling is one of the early signs of the condition, which can occur without having an obvious injury to the site.
Sign UP
Sign up for your free trial now!
Get started with Rehab My Patient today and revolutionize your exercise prescription process for effective rehabilitation.
Start Your 14-Day Free Trial